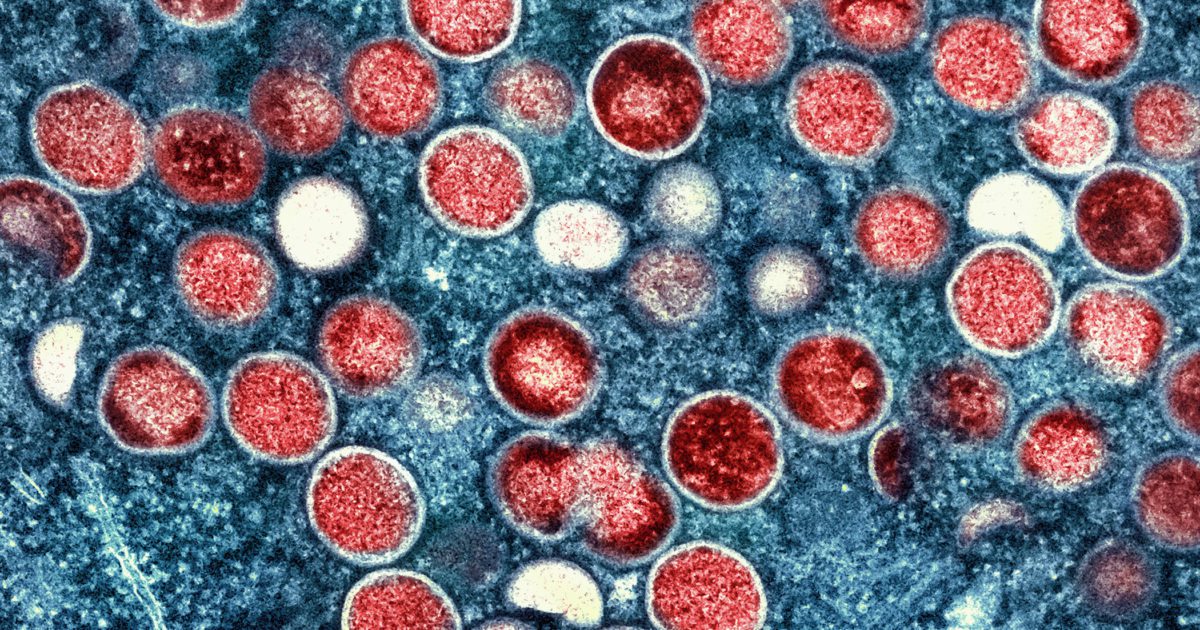
A case study published in the JACC: Case Reports found that a 31-year-old man with a confirmed monkeypox infection developed acute myocarditis one week after first showing symptoms.
Unsurprisingly, scientists are already saying that monkeypox can result in cardiac complications like myocarditis.
Myocarditis is inflammation of the heart muscle, typically caused by a viral infection.
A patient w/ #Monkeypox developed acute #myocarditis confirmed by CMR.
This case highlights cardiac involvement as a potential complication associated w/ Monkeypox. Further monitoring needed for recognition of other future complications. https://t.co/UO48zV4JzW #JACCCaseReports pic.twitter.com/PqR83frKQm
— JACC Journals (@JACCJournals) September 2, 2022
https://twitter.com/mildanalyst/status/1565884972086562817
However, an obvious elephant in the room remains unanswered.
Did the patient receive the COVID-19 shot?
It’s also worth asking if the patient had the monkeypox (smallpox) shot.
Myocarditis from monkeypox! 🤦🏼♀️ couldn’t have anything to do with the poison ☠️💉💉💉 pic.twitter.com/dNRS7nVfGN
— AB (@bonomi_a) September 5, 2022
From 9 News:
The lead author of the study, Dr Ana Isabel Pinho, said the case highlighted cardiac involvement as a potential complication associated with monkeypox infection.
“We believe that reporting this potential causal relationship can raise more awareness of the scientific community and health professionals for acute myocarditis as a possible complication associated with monkeypox,” she said.
The study found the patient presented to a health clinic five days following the onset of monkeypox symptoms, including malaise, myalgia, fever and multiple swollen lesions on the face, hands and genitalia.
After a PCR swab sample of a skin lesion, it was confirmed the man had a positive monkeypox infection.
The patient returned to the emergency department three days later, reporting chest tightness radiating through his left arm.
News Medical Life Sciences provided additional details:
The patient had a mild infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) two months before the diagnosis of monkeypox infection. In addition, he was treated with pre-exposure prophylaxis against human immunodeficiency virus (HIV) due to sexual risk exposure (men who have sex with men).
Except for tobacco use and occasional cannabis use, he did not mention consuming any other illicit drugs or alcohol.
Clinical investigations
The electrocardiography (ECG) findings of the patient revealed ventricular repolarization abnormalities. However, a normal cardiothoracic index was observed in the chest x-ray examination. Regarding biochemical parameters, increased levels of C-reactive protein, creatine phosphokinase, troponin I, and brain natriuretic peptide were observed.
Based on the clinical findings, the patient was suspected of having acute myocarditis (heart muscle inflammation) and was admitted to the intensive care unit under airway isolation. After 24 hours of admission, cardiac magnetic resonance was performed, which revealed myocardial inflammation, edema, and necrosis. Based on these findings, the diagnosis of acute myocarditis was confirmed.
The patient was treated with supportive care and exercise restriction and had a complete clinical recovery. The treatment with non-steroidal anti-inflammatory drugs was terminated.
Significance
This case report highlights the possibility of cardiac manifestations in patients with monkeypox infection. This finding might help physicians to make appropriate diagnostic and therapeutic decisions.
Both monkeypox and smallpox viruses belong to the orthopoxvirus family. Although more aggressive than monkeypox infection, smallpox infection is known to associate with myocarditis. Cardiac complications have also been noticed in individuals immunized with smallpox vaccines. Thus, being a related virus, monkeypox may also have a tropism for cardiac tissue, justifying the incidence of acute myocarditis in a monkeypox-infected patient.
Read the JACC: Case Report HERE.

Join the conversation!
Please share your thoughts about this article below. We value your opinions, and would love to see you add to the discussion!